Previous research has shown significant differences in glycemic control between women and men living with diabetes. At the ATTD conference, lectures dedicated to the challenges women face in everyday life with diabetes were held on International Women’s Day itself.
Type 1 diabetes is demanding on its own—more than 40 factors influence glucose levels—and when the monthly hormonal cycle in women is taken into account, management becomes even more complex. Different phases of the menstrual cycle affect insulin sensitivity, making it harder to maintain a satisfactory Time in Range (TIR). The IMAGINE (dIabetes MAnaGment IN womEn) study is a large-scale investigation into the quality of diabetes control in men and women and identifies additional difficulties women experience depending on different phases of the cycle.
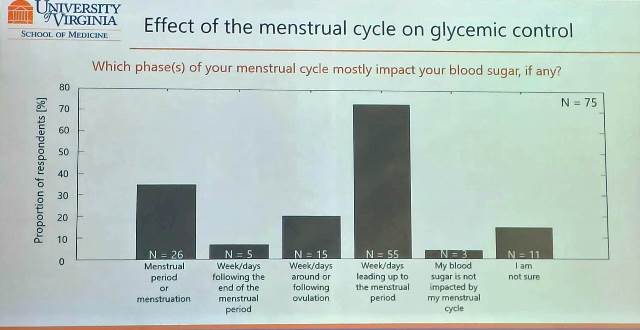
So far, the study has shown that for most women included (as many as 73%), the largest changes in blood glucose levels—specifically a tendency toward hyperglycemia—occur in the week or several days before menstruation.
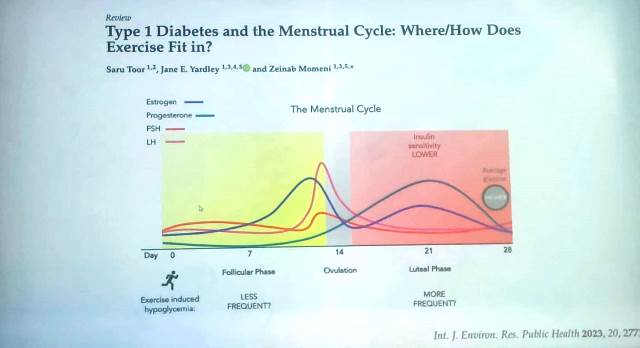
In addition, the highest incidence of hypoglycemia has been observed during menstruation and in the middle of the follicular phase. This is logical, as insulin sensitivity increases during the follicular phase, which begins on the first day of menstruation, and women generally require less insulin. This creates a problem for AID (automated insulin delivery) systems—hybrid closed-loop systems—because pumps are often unable to recognize changes in insulin sensitivity quickly enough. As a result, women inevitably receive incorrect insulin delivery during part of the cycle, placing them at higher risk of hypoglycemia during menstruation or causing elevated glucose levels immediately before menstruation.
The IMAGINE study highlights the need for improved technological solutions that can account for hormonal changes throughout the cycle. Clinical trials have been announced and began in the summer of 2024, with the goal of developing insulin therapy adaptation strategies that better track metabolic changes associated with these hormonal fluctuations.
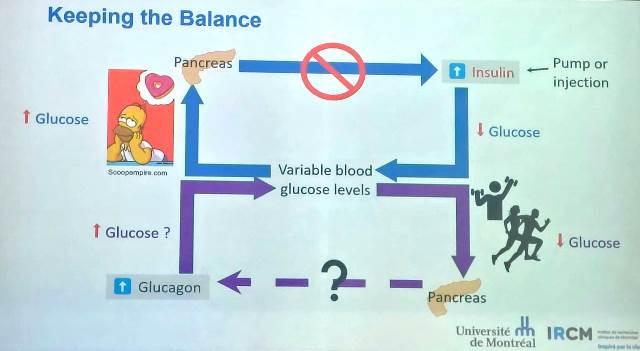
Another challenge affects all people with diabetes, not just women: how to exercise with diabetes. An excellent lecture was given by Dr. Jane Yardley, who emphasized that “exercise with diabetes is more art than science.” The body of a healthy person has a perfectly precise mechanism that continuously regulates insulin secretion by the pancreas and glucagon release, adjusting both according to blood glucose concentration.
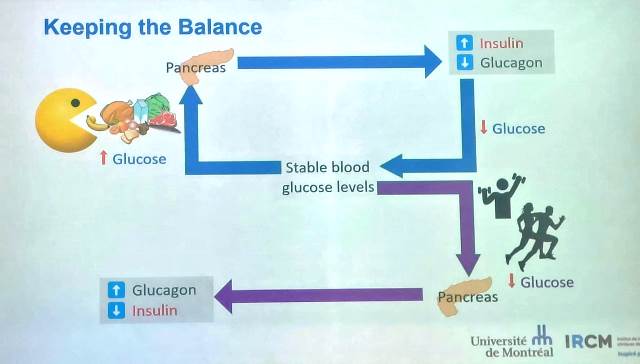
In people with diabetes, even when relying on CGM and AID systems, and despite the fastest-acting synthetic insulins, such precise and rapid responses are currently not possible. During physical activity—especially unplanned exertion—there is often a risk of hypoglycemia. Exercise itself is demanding, and the additional stress and fear of hypoglycemia discourage people with type 1 diabetes from exercising, even though physical activity is crucial for maintaining quality of life.
On average, women with type 1 diabetes are less physically active than men, possibly due to a greater fear of hypoglycemia and loss of diabetes control, to which they are more susceptible because of hormonal influences on glycemia. This issue is further compounded by the fact that current guidelines for insulin dose adjustment during exercise are based on studies conducted exclusively in men, indicating a clear need for further work in this area. At present, it is known that exercising during the luteal phase is “riskier” in terms of hypoglycemia because higher insulin doses are typically required due to reduced insulin sensitivity, while physical activity itself increases insulin sensitivity, making low glucose levels more likely.
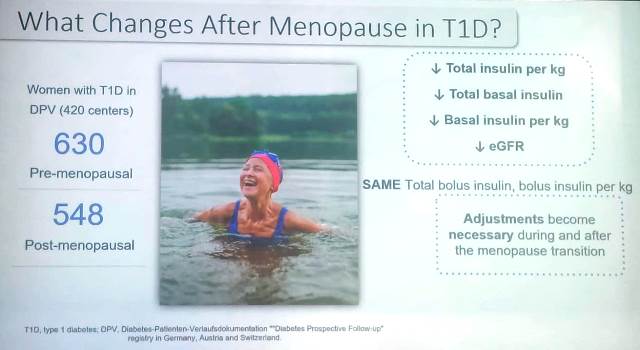
A particularly under-researched area involves women with type 1 diabetes during menopause. In addition to numerous hormonal changes, menopause is associated with a reduced need for basal insulin and a lower total daily insulin requirement, while bolus insulin needs on average remain unchanged, making dose adjustments necessary. Compared with healthy women, women with type 1 diabetes in menopause have a higher risk of fractures, lose muscle mass more rapidly, and have an increased cardiovascular risk.
What is certain is that exercise and physical activity, at any age, lead to better vascular health, increased insulin sensitivity, higher bone density, improved muscle quality and strength, and better mobility—regardless of age or sex.
Author: Mirna