Someone who is not well-acquainted with diabetes and its treatment might think that pancreas transplantation is a simple and definitive solution. If the problem is a pancreas that does not produce insulin or produces it insufficiently, why not simply transplant a new pancreas and solve the issue once and for all? Unfortunately, things are not that simple.
What is a pancreas transplant?
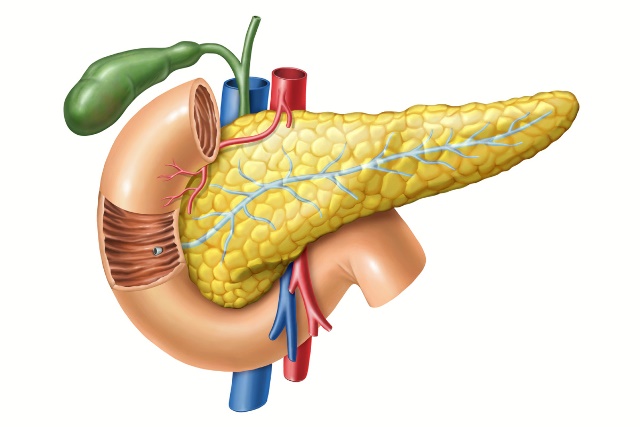
A pancreas transplant is a complex medical procedure in which a patient receives a new pancreas from a deceased donor. This procedure is most commonly performed on people with type 1 diabetes, and only in specific cases.
The pancreas is an organ that plays a key role in insulin production—the hormone that regulates blood sugar levels. In type 1 diabetics, the immune system attacks and destroys the insulin-producing cells, leading to a lifelong need for insulin therapy. In theory, a transplant could restore the natural insulin function.

Why isn’t it an option for everyone?
Although this sounds promising, there are several reasons why pancreas transplantation is not a standard solution for all diabetics:
1. Risk of organ rejection
Like any organ transplant, there is a significant risk that the patient's body will reject the new organ. To prevent this, patients must take immunosuppressive drugs for the rest of their lives. These drugs weaken the immune system, making patients more susceptible to infections and increasing the risk of other serious complications.
2. Surgical complications
A pancreas transplant is a major surgical procedure that carries risks such as bleeding, infections, and damage to other organs. The surgery is not always successful, and failure can lead to serious consequences.
3. Lack of donors
There is a saying that spring is the best time for a pancreas transplant because many motorcyclists take to the roads after a long winter and, unprepared, suffer fatal accidents. In other words, a pancreas can only be obtained from a deceased suitable donor, meaning that organ availability is very limited. Priority for transplantation is usually given to patients with severe diabetes complications, such as kidney failure, rather than those who manage their condition well with insulin therapy.
4. Immunosuppressive drugs are risky
While a pancreas transplant can free a patient from insulin injections, lifelong immunosuppressive therapy comes with many risks. Long-term use of these drugs can cause kidney damage, an increased risk of cancer, and serious infections.
5. Not suitable for type 2 diabetes
Type 2 diabetes is usually not caused by a lack of insulin but by the body's resistance to insulin. Therefore, a pancreas transplant would not solve the problem since the root of the disease lies in metabolic processes rather than in the pancreas itself.

When is a pancreas transplant recommended?
Pancreas transplantation is most commonly performed on type 1 diabetics who also have severe kidney damage and need a kidney transplant. In such cases, simultaneous pancreas-kidney transplantation (SPK) is often performed. In these situations, the benefits of transplantation may outweigh the risks.
Conclusion
Although a pancreas transplant might seem like a "magical solution" for diabetes, the reality is much more complex. The risks associated with surgery, lifelong immunosuppressive therapy, and limited organ availability make this option suitable only for a small number of patients with the most severe complications. For most diabetics, proper disease management through insulin therapy, a healthy diet, and physical activity remains the best way to lead a quality life.